Background: Infection during the period of neutropenia following chemotherapy represents a major cause of morbidity and mortality in patients with malignancy.(Freifeld, et al, 2011, Baden LR, et al, 2012) Several guidelines recommend granulocyte colony stimulating factor (GCSF) to reduce the duration and severity of chemotherapy-induced neutropenia and abate infection risk.(Lyman, et al 2018, Aapro, et al, 2011, Smith, et al, 2015). Optimal GCSF administration following chimeric antigen receptor (CAR) T-cell therapy remains undefined and requires characterization.
Methods: The Mayo Institutional Review Board approved this retrospective, single-center study. Electronic medical records for patients prescribed axicabtagene ciloleucel were reviewed until disease relapse, death, or a maximum of 60 days after infusion. Baseline characteristics and laboratory values were abstracted prior to lymphodepleting chemotherapy. GCSF support was originally prescribed when the absolute neutrophil count (ANC) declined below 500 cells/mm3 and discontinued when the ANC exceeded 1000 cells/mm3 (neutropenia) for 2 consecutive days. A practice change was made where GCSF was recommended only in those with febrile neutropenia and an increased concern for infection. The primary endpoint was the difference in the total days of neutropenia for patients receiving and not receiving GCSF. Secondary outcomes compared total days of severe neutropenia, number of neutropenia episodes, infection rates by GCSF use, and outcomes by protocol change. Neutropenia and severe neutropenia were defined as an ANC below 500 cells/mm3 and 100 cells/mm3, respectively. Updated data with more patients will be presented at the conference.
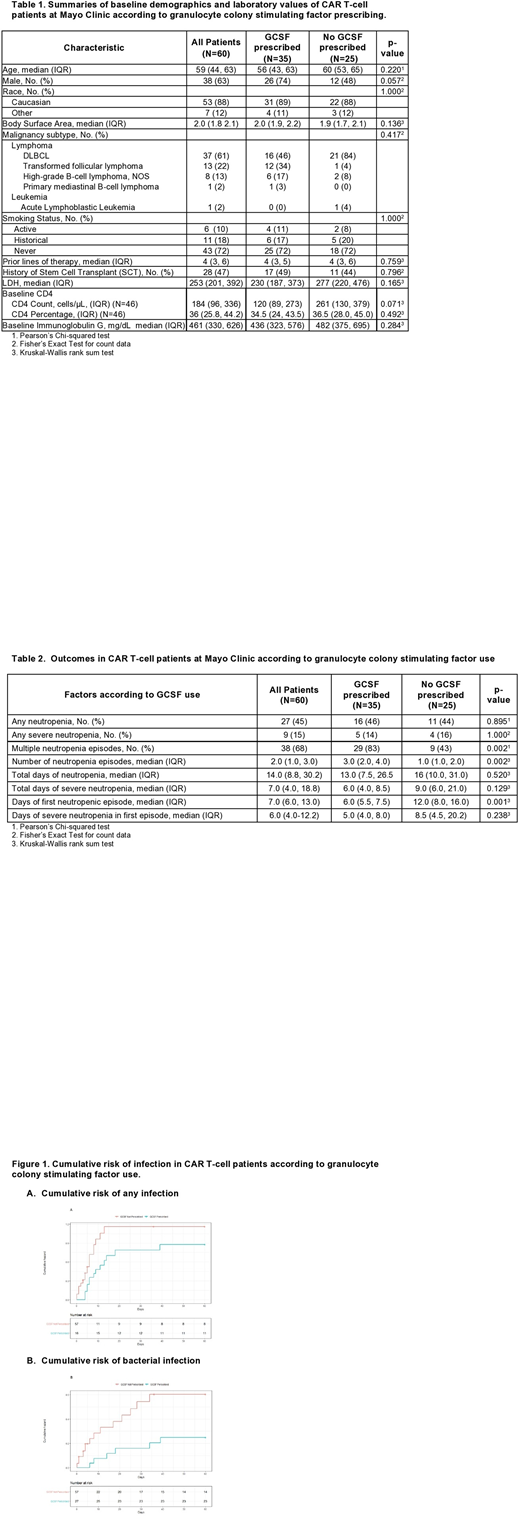
Results: The 60 included patients had a median age of 59 (IQR: 44, 63) years, 38 (63%) were male and 53 (88%) were Caucasian. Significantly fewer patients were prescribed GCSF according to infection-related concerns compared to ANC-based indication, 18% vs. 94%, p<0.001. Because only 3 subjects received GCSF based on infection-related concerns, results based on GCSF use versus no use is shown here. GCSF was prescribed to 35 (58%) patients for a median of 8 (IQR: 6, 12) doses with a median cumulative dosage of 3840 mcg (IQR 2100-5400) and median time to first dose of 3 days (IQR: 1, 4) post CAR T-cell infusion. Table 1 displays additional baseline characteristics and laboratory parameters according to GCSF support utilization.
GCSF prescribed: Table 2 displays outcomes by GCSF use. Total days of neutropenia were similar between groups (13 vs. 16, p=0.52) with a trend towards significantly fewer days of severe neutropenia when prescribed GCSF (6 vs. 9, p=0.129). Patients prescribed GCSF were more likely to experience multiple episodes of neutropenia (83% vs. 43% p=0.002) with a significantly greater median number of episodes (3 vs. 1, p=0.002) when compared to those not prescribed GCSF. GCSF use significantly decreased the median days of the first neutropenia episode (6 vs. 12, p=0.001). There was a trend for decreased median days of severe neutropenia in the first episode with GCSF (5.0 vs. 8.0, p=0.236). Figure 1 displays a trend towards a lower overall risk of infection (HR 0.55, 95%CI: 0.16-1.87, p=0.34) and lower risk of bacterial infection (HR: 0.49, 95% CI: 0.18-1.31, p=0.15); however, these were not statistically significant.
Conclusion: Patients prescribed GCSF according to ANC-based indication were significantly more likely to experience multiple neutropenia episodes; however, duration of first neutropenic episode and days of severe neutropenia during the first neutropenic episode were significantly reduced. Interestingly, the total days of neutropenia and severe neutropenia were similar between groups. It is possible that using the parameter of ANC more than 1000 cells/mm3 for 2 consecutive days is not the optimal criteria for stopping GCSF. Risk of overall and bacterial infection was lower with ANC-based initiation of GCSF, although non-significant likely due to small sample size. The potential benefit for using CSF and the optimal timing after CAR T-cell infusion requires further, rigorous, prospective investigation.
Ansell:ADC Therapeutics: Research Funding; Trillium: Research Funding; Affimed: Research Funding; Regeneron: Research Funding; AI Therapeutics: Research Funding; Takeda: Research Funding; Seattle Genetics: Research Funding; Bristol Myers Squibb: Research Funding. Bennani:Purdue Pharma: Other: Advisory Board; Kite/Gilead: Research Funding; Affimed: Research Funding; Verastem: Other: Advisory Board. Lin:Kite, a Gilead Company: Consultancy, Research Funding; Vineti: Consultancy; Sorrento: Consultancy, Membership on an entity's Board of Directors or advisory committees; Gamida Cells: Consultancy; Takeda: Research Funding; Merck: Research Funding; Legend BioTech: Consultancy; Juno: Consultancy; Bluebird Bio: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Novartis: Consultancy; Janssen: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal